Publication by CIRI in the journal EMBO Molecular Medicine on October 7, 2019.
Familial Mediterranean fever (FMF) is the most frequent hereditary systemic autoinflammatory syndrome. FMF is usually caused by bi-allelic mutations in the MEFV gene, encoding Pyrin. Conclusive genetic evidence lacks for about 30% of patients diagnosed with clinical FMF. Pyrin is an inflammasome sensor maintained inactive by two kinases (PKN1/2). The consequences of MEFV mutations on inflammasome activation are still poorly understood. Here, we demonstrate that PKC superfamily inhibitors trigger inflammasome activation in monocytes from FMF patients while they trigger a delayed apoptosis in monocytes from healthy donors. Expression of the pathogenic p.M694V MEFV allele is necessary and sufficient for PKC inhibitors (or mutations precluding Pyrin phosphorylation) to trigger caspase-1- and gasdermin D-mediated pyroptosis. In line with colchicine efficacy in patients, colchicine fully blocks this response in FMF patients' monocytes. These results indicate that Pyrin inflammasome activation is solely controlled by Pyrin (de)phosphorylation in FMF patients while a second control mechanism restricts its activation in healthy donors/non-FMF patients. This study paves the way towards a functional characterization of MEFV variants and a functional test to diagnose FMF.
 The problem: Familial Mediterranean Fever (FMF) is the most frequent hereditary systemic auto-inflammatory disease. FMF is, in most cases, associated with bi-allelic mutations of the MEFV gene encoding Pyrin, an inflammasome sensor. The link between MEFV mutations and the dysregulated Pyrin inflammasome activation observed in FMF patients is unclear. Furthermore, most of the 365 described MEFV variants are of uncertain significance and the genetic validation of the clinical FMF diagnosis remains challenging.
The problem: Familial Mediterranean Fever (FMF) is the most frequent hereditary systemic auto-inflammatory disease. FMF is, in most cases, associated with bi-allelic mutations of the MEFV gene encoding Pyrin, an inflammasome sensor. The link between MEFV mutations and the dysregulated Pyrin inflammasome activation observed in FMF patients is unclear. Furthermore, most of the 365 described MEFV variants are of uncertain significance and the genetic validation of the clinical FMF diagnosis remains challenging.
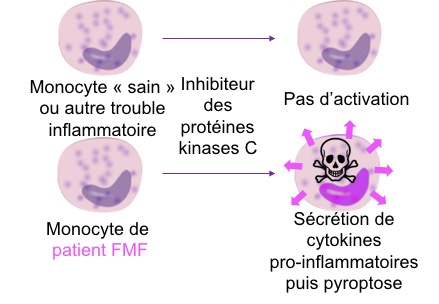
The results: Thanks to the use of protein kinase inhibitors and phosphonull mutants, this study demonstrates that Pyrin dephosphorylation triggers full inflammasome activation in FMF patients monocytes but not in healthy donors' monocytes. Furthermore, the pathogenic p.M694V MEFV mutation, most frequently observed in FMF patient, triggers constitutive inflammasome activation only when combined to phosphonull MEFV mutations. These results indicate that Pyrin inflammasome activation is controlled by two independent mechanisms in healthy donors but only by phosphorylation/dephosphorylation in FMF patients. This difference can be exploited using protein kinase inhibitors and primary monocytes from patients to functionally diagnose FMF.
Clinical impact: This study increases our knowledge of the molecular mechanisms underlying inflammation in FMF patients. Furthermore, it should improve FMF diagnosis by providing a quick and easy test in primary monocytes to discriminate FMF patients from patients with unrelated inflammatory conditions. Finally, this study provides means to determine the pathogenicity of MEFV variants, which should reduce in the future the number of variants of uncertain significance and improve genetic testing.
Source: Pyrin dephosphorylation is sufficient to trigger inflammasome activation in Familial Mediterranean Fever patients. Flora Magnotti, Lucie Lefeuvre, Sarah Benezech, Tiphaine Malsot, Louis Waeckel, Amandine Martin, Sébastien Kerever3, Daria Chirita, Marine Desjonqueres, Agnès Duquesne, Mathieu Gerfaud-Valentin, Audrey Laurent, Pascal Sève, Michel-Robert Popoff, Thierry Walzer, Alexandre Belot, Yvan Jamilloux, Thomas Henry. EMBO Mol Med (2019)11:e10547






